AI & Healthcare: challenges, innovations and improving quality of life

Table of contents
- Current situation: what is AI in healthcare today?
- From raw data to personalised care: the key role of AI
- The challenge of adherence: wearables, gamification and the human factor
- The essential role of carers in the digital ecosystem
- Developing an AI solution in healthcare: the four pillars of success
- FAQ: AI in Healthcare
- Transform your vision into a truly engaging AI healthcare solution
AI in healthcare is no longer limited to fundamental research or surgical robotics. From diagnostic assistance via machine learning to patient-centred digital medical devices (DMNs), it is redefining the care pathway. Machine learning algorithms now analyse millions of medical images to detect cancer, while health data is transforming reactive medicine into predictive medicine.
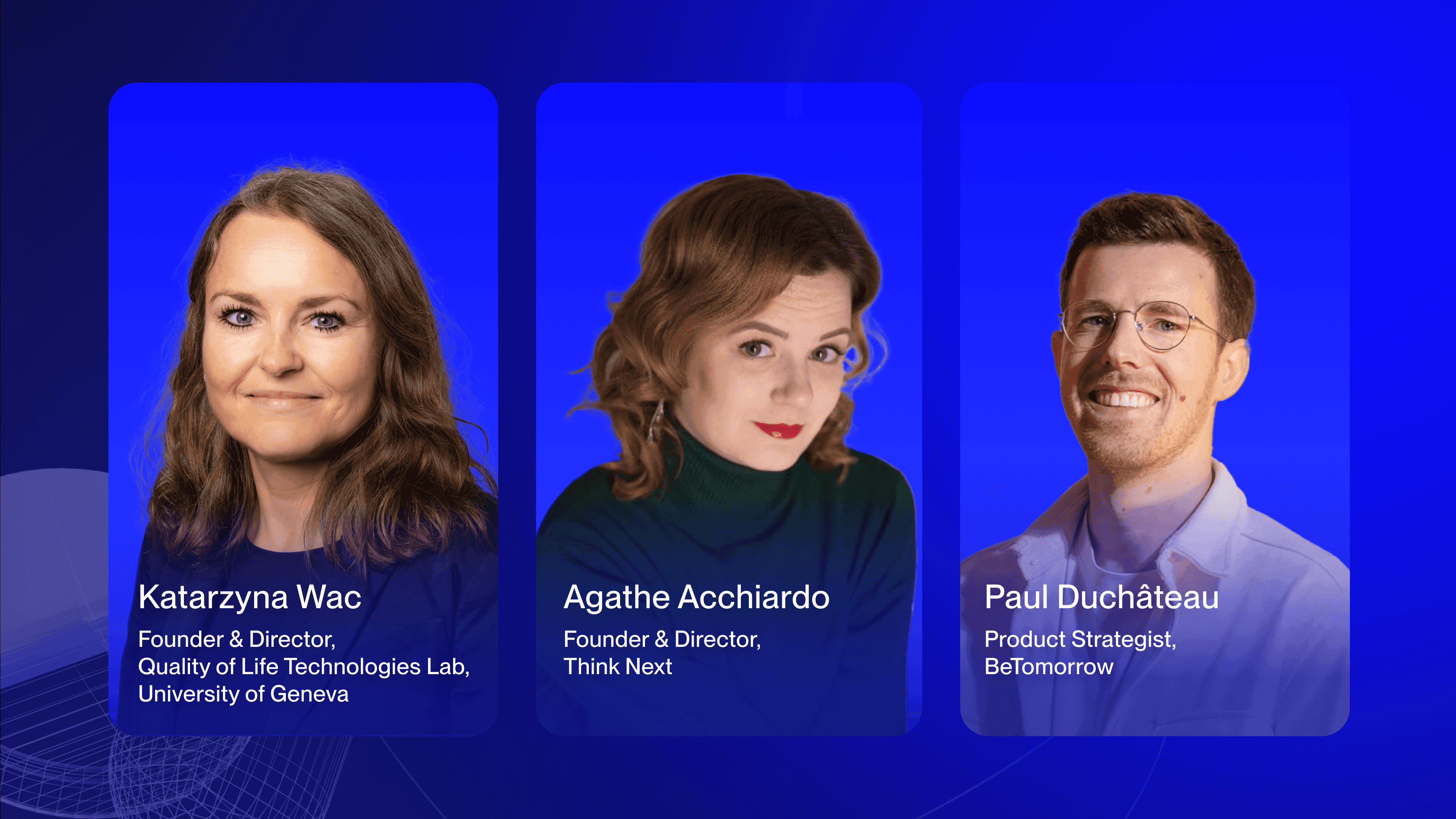
But beyond pure technological performance, a major challenge is emerging: how can artificial intelligence tangibly improve patients' daily quality of life? How can we move from "treating" to "living better"? We take a look at the strategic challenges and opportunities for e-health players, based on our expertise and the BeTomorrow webinar "Digital Health: Augment Quality of Life with AI".

Current situation: what is AI in healthcare today?
The three technological pillars transforming medicine
Artificial intelligence in healthcare is currently based on three major areas of application, each responding to distinct clinical needs:
1. Algorithm-assisted diagnosis
Deep learning systems excel at analysing medical imaging. Trained on millions of X-rays, CT scans and MRIs, these predictive algorithms detect anomalies that the human eye might miss. In dermatology, for example, some models achieve accuracy rates comparable to those of experienced dermatologists in identifying melanomas. An algorithm does not "guess". It identifies statistical patterns in massive datasets. This is why the quality of the training data determines its clinical reliability.
2. Predictive and personalised medicine
Thanks to big data and digital biomarkers, AI can now anticipate the risk of chronic diseases before symptoms appear. Predictive models combine genetics, medical history, behaviour (via wearables) and environmental factors to establish individualised risk scores. This precision medicine allows intervention at the preventive stage rather than the acute stage.
3. Robotics and medical assistance
In the operating theatre, AI-assisted robotic systems increase surgeons' precision. In nursing homes, conversational robots using language models (such as ChatGPT) combat isolation among the elderly. These technologies do not replace humans: they extend their capabilities.
The regulatory and ethical framework: a necessary step
Developing an AI solution for healthcare in France involves navigating a strict regulatory environment:
HAS (Haute Autorité de Santé): Evaluates digital medical devices for potential reimbursement. A diagnostic algorithm must prove its clinical usefulness through robust studies.
GDPR and data security: Health data is sensitive. Its processing requires certified infrastructure (HDS-approved hosts) and full traceability of data flows.
AI ethics: Algorithmic bias (over-representation of a population in training data) can create inequalities in care. Transparency and explainability (explainable AI) are becoming imperative.
Caution: An algorithm that performs well in the laboratory may fail in real-world conditions if its framework for use has not been designed in consultation with healthcare professionals and patients.
From raw data to personalised care: the key role of AI
Transforming big data into actionable insights
AI in healthcare excels in one specific area: extracting meaning from informational chaos. A chronic patient generates thousands of data points every month (blood sugar, blood pressure, physical activity, sleep, medication adherence). Analysing these flows manually? Impossible. This is where machine learning algorithms come in.
As Agathe ACCHIARDO, our webinar guest and founder of Think Next (a consulting firm specialising in foresight and innovation in the healthcare sector) points out:
“AI must go beyond simply reminding patients to take their medication. It must provide personalised recommendations based on the analysis of individual behaviours, to enable patients to live better with their chronic conditions.”
In concrete terms, an effective AI system transforms:
Raw data (e.g., glucose at 1.8 g/L at 11 p.m. after a carbohydrate-rich meal)
Into actionable insights ("Your night-time blood sugar spikes are linked to your late dinners. Try to eat dinner before 8 p.m. this week.")
This ability to contextualise, personalise and anticipate distinguishes a mediocre e-health solution from a truly effective digital care pathway.
Real-world use case: the example of Toilet Finder
The most impactful innovations are not always the most technological. The Toilet Finder app, developed by BeTomorrow, perfectly illustrates how AI in healthcare can improve quality of life through pragmatic solutions.
Initially designed to integrate GPS functionality and indicate the location of public toilets, this app has gained an unexpected use for patients suffering from chronic intestinal diseases (Crohn's, ulcerative colitis) or endometriosis. By facilitating quick access to suitable toilets, it reduces:
Social anxiety: The fear of not finding a toilet limits outings. The app restores a form of autonomy.
Barriers to employment: Some patients avoid jobs that require travel.
Isolation: Being able to go out with peace of mind improves social participation.
This example highlights the importance for personalised medicine companies to create solutions that meet practical and immediate needs, while offering measurable long-term benefits. Unlike assisted diagnosis applications that target healthcare professionals, this type of solution directly targets patients in their "real life" (Real World Evidence concept)

ARTIFICIAL INTELLIGENCE: 5 USE CASES IN THE HEALTHCARE SECTOR
- Advances in customized medicine, optimized by artificial intelligence.
- The benefits of AI for caregivers and patients.
- The power of AI to anticipate disease through data analysis.
- The capabilities of AI to optimize the management of medical resources and processes.
The challenge of adherence: wearables, gamification and the human factor
Why 70% of connected devices end up in a drawer
You're probably familiar with this scenario: a patient receives their wearable device (smartwatch, continuous glucose monitor, connected blood pressure monitor). The first three weeks? Enthusiasm and compulsive data checking. After three months? The device is gathering dust in a drawer.

Katarzyna WAC, Director of the Quality of Life Technologies Lab at the University of Geneva, and our second speaker on the webinar, explains this phenomenon:
“Patients don't just want to collect data. They want that data to help them feel better and improve their daily lives. Without a tangible perceived benefit, patient engagement collapses.”
There are many reasons for this massive dropout rate:
Lack of personalisation: Alert thresholds are generic and not tailored to individual profiles.
Lack of positive feedback: The app does not highlight progress, it simply displays figures.
Information overload: Too many notifications kill the notification. The patient becomes desensitised
Disconnection from the care pathway: Data is not shared with the doctor, who continues to base their decisions on quarterly consultations.
Gamification as a lever for therapeutic engagement
Faced with this challenge of compliance, health gamification is emerging as a proven solution. The principle? Borrow the mechanics of video games (progression, rewards, challenges) to maintain long-term engagement.
The 5 gamification mechanisms that work in healthcare:
Progress visualisation: 3-month trend graphs (not just the latest value). Patients can see the concrete impact of their efforts.
Points and badge system: Reward daily adherence (e.g. "7 consecutive days of taking your blood pressure in the morning").
Progressive challenges: Set gradual goals ("Walk 500 more steps this week") rather than unattainable goals.
Social dimension: Groups of patients sharing common challenges (with anonymisation if necessary).
Feed-forward, not just feedback: AI predicts the impact of future behaviours ("If you maintain this walking pace, your HbA1c should drop by 0.3% within 2 months").
Gamification does not replace therapeutic effectiveness. It is an adherence booster. A fun game that does not improve health remains a game, not a digital medical device.
Agathe Acchiardo emphasises this point:
“Patients need to be able to visualise their progress over time in order to feel a sense of personal effectiveness and be motivated to use the app in the long term.”

The essential role of carers in the digital ecosystem
A common strategic error in the development of digital health products? Designing solely for the patient. In reality, 60% of chronically ill patients rely on at least one carer (spouse, parent, child) for the day-to-day management of their illness.
Carers are often the real users of e-health solutions:
They configure the application.
They check alerts.
They encourage (or enforce) regular use.
Katarzyna Wac points out that the cognitive and emotional burden on carers is systematically underestimated by digital solution designers. The result? Overly complex interfaces, anxiety-inducing notifications, and a lack of dedicated features.
How to integrate carers into your product strategy?
Create a dual account: Patient + Carer, with different access levels.
Provide dedicated insights: "Your loved one has taken their medication correctly this week" (reassurance) vs "3 abnormal blood sugar spikes detected" (actionable alert).
Offer support resources: AI in healthcare can also be used to reduce caregiver burnout by automating repetitive tasks (reminders, appointment tracking).
Artificial intelligence adds an extra dimension by automating certain repetitive tasks and providing accurate recommendations, thereby reducing the mental load on caregivers while improving the effectiveness of care.
Developing an AI solution in healthcare: the four pillars of success
Are you a pharmaceutical company, a MedTech start-up or a digital health player? Here are the key success factors identified by industry experts to maximise the adoption and impact of your solution.
1. Adopt a human-centred approach, not a patient-centred one
This is a major semantic nuance. In the collective imagination, a "patient" is an individual defined by their illness, passive and hospitalised. A "human" lives, works, loves and travels, with a chronic illness in the background.
As Katarzyna Wac explains:
“It is crucial to model the real behaviours and needs of individuals in their everyday context, rather than focusing solely on traditional clinical parameters.”
In concrete terms, this means:
Measuring quality of life, not just biomarkers. Perfect HbA1c but a destroyed social life is not a therapeutic success.
Designing for "healthspan", not just "lifespan". The goal is not to live 90 years bedridden, but 85 years independently.
Integrating Patient-Reported Outcomes (PROs): Only the patient can describe the real impact of a symptom on their life.
2. Practice co-design with all stakeholders
An e-health solution can only be successful if it is integrated into a complex ecosystem:
Patients and carers: To ensure real usability.
Doctors and healthcare professionals: To ensure clinical credibility and integration into the care pathway.
Payers (Social Security, mutual insurance companies): To obtain reimbursement via the HAS.
Co-design involves regular workshops from the prototype phase onwards, not retrospective validation. User experience (UX) design methodologies adapted to healthcare (such as medical Design Thinking) are essential.

3. Ensure regulatory compliance from the design stage onwards.
AI in healthcare operates within a strict regulatory framework. Integrating compliance at the end of a project means running the risk of having to start all over again.
The three regulatory aspects to anticipate:
Classification as a DMN (Digital Medical Device): If your solution diagnoses, monitors or treats, it is considered a medical device. CE marking is mandatory.
GDPR compliance and HDS hosting: Health data must be hosted on certified servers. Data processing and security are non-negotiable.
HAS assessment for reimbursement: Document clinical utility through studies (ideally randomised) from the pilot phase onwards.
Please note: Scalable AI algorithms (which learn during production) pose specific regulatory challenges. The CE-certified version must remain fixed or follow a validated update protocol.
4. Build a viable business model
Technological enthusiasm is not enough. An AI solution in healthcare must generate economic value to be sustainable.
Three possible financing models:
B2B via pharmaceutical companies: Develop a companion app for a chronic medication (improved compliance).
B2B via mutual insurance companies: Offer prevention programmes that reduce long-term care costs.
Direct reimbursement by the National Health Service: The Holy Grail, but requires a long and costly HAS validation process.
The population is ageing and chronic diseases are skyrocketing. The shift from an approach focused on longevity to one focused on quality of life is not a passing trend. It is a structural transformation of the healthcare system.
FAQ: AI in Healthcare
What exactly is AI in healthcare?
AI in healthcare refers to all artificial intelligence technologies (machine learning, deep learning, natural language processing) applied to the medical sector. It covers assisted diagnosis, predictive medicine, personalised treatment, optimisation of care pathways and improvement of patients' quality of life through digital medical devices.
What are the main uses of AI in healthcare?
The three main areas are: 1) Diagnostic assistance (medical imaging analysis, cancer detection), 2) Personalised medicine through Big Data analysis (risk prediction, dosage adjustment), 3) Patient-centred e-health solutions (wearables, therapeutic applications, gamification for compliance).
How does AI improve patients' quality of life?
AI in healthcare transforms raw health data into actionable insights. For example, instead of simply displaying a blood sugar level, an AI system identifies patterns ("Your spikes occur after high-carbohydrate meals in the evening") and suggests concrete behavioural adjustments. It also helps reduce anxiety through practical tools (e.g. apps that locate toilets for people with chronic illnesses).
What is a Digital Medical Device (DMD)?
A DMN is an application or software programme considered to be a medical device because it diagnoses, monitors or treats a medical condition. In France, these solutions must obtain CE marking and may be evaluated by the HAS for potential reimbursement. Predictive algorithms used in healthcare often fall into this category.
Why do patients abandon health applications?
70% of wearables and applications are abandoned after 3 months. The main reasons are: lack of personalisation, lack of positive feedback highlighting progress, overload of notifications, and above all, lack of perceived tangible benefits in terms of quality of life. This is why health gamification and a human-centred approach are becoming essential.
How can AI be integrated into healthcare in compliance with the GDPR?
Health data is sensitive data. Processing it requires: 1) HDS (Health Data Host) certified hosting, 2) the patient's explicit consent, 3) full traceability of access and processing, 4) anonymisation or pseudonymisation of data for training machine learning algorithms. Data processing and security must be considered from the design stage (Privacy by Design).
What is the role of carers in e-health solutions?
Carers (family, loved ones) are often the real everyday users of AI solutions in healthcare for chronic patients. They configure settings, check alerts and encourage use. Integrating them into the product strategy (dual Patient/Carer accounts, dedicated insights, automation of repetitive tasks) drastically improves adherence and reduces their mental load.
How can a company develop a profitable AI healthcare solution?
Four pillars: 1) Co-design with patients, carers and payers from the outset, 2) Anticipated regulatory compliance (DMN, GDPR, HAS), 3) Evidence of clinical and economic effectiveness (randomised studies), 4) Viable business model (B2B laboratories/mutual insurance companies or National Health Service reimbursement). The approach focused on healthspan (quality of life) rather than simply treatment differentiates successful solutions.
Transform your vision into a truly engaging AI healthcare solution
Artificial intelligence in healthcare is not an end in itself. It is a powerful tool, but one that only creates value when used to serve a humanistic vision: improving not the performance of an algorithm, but the real daily lives of millions of patients and carers.
The convergence of personalised medicine, gamification, big data analysis and user experience design opens up unprecedented opportunities. But it also requires rare multidisciplinary expertise: technical mastery of machine learning algorithms, understanding of the regulatory framework (HAS, GDPR), and above all, the ability to design for humans, not for "abstract patients".
Are you developing a Digital Medical Device or an e-health solution?
Talk to our experts in Data, AI and UX Design specialising in the healthcare sector. We support pharmaceutical companies, MedTech start-ups and digital health players to maximise the adoption and clinical impact of their solutions.
For example, we collaborated with Biogen, an international healthcare and biotechnology company, to resume development of its Cleo app, a digital companion for people with multiple sclerosis.
Contact our experts in AI and digital health
Watch the full presentations by Katarzyna Wac (University of Geneva) and Agathe Acchiardo (Think Next) on patient engagement strategies and the integration of AI into care pathways: Watch the webinar replay
Cet article, initialement publié en octobre 2024, a été mis à jour le 8 janvier 2026 afin d’intégrer un panorama élargi de l’IA en santé, les enjeux réglementaires actuels et les enseignements du webinaire BeTomorrow.


